Publisher: ScienceDirect
Authors: A. Chiorean, S. Kabadi, P. Hayat, M. Montmerle, E. Ponce, M. Blanchon, N. Lyn, M. Maski
Date: 7–11 February 2022
DOI: doi.org/10.1016/j.ymgme.2021.11.063
CONFERENCE/VALUE IN HEALTH INFO:
N°48, 2022-02, Presented at WORLD Symposium 2022, San Diego, CA, USA
ABSTRACT
INTRODUCTION:
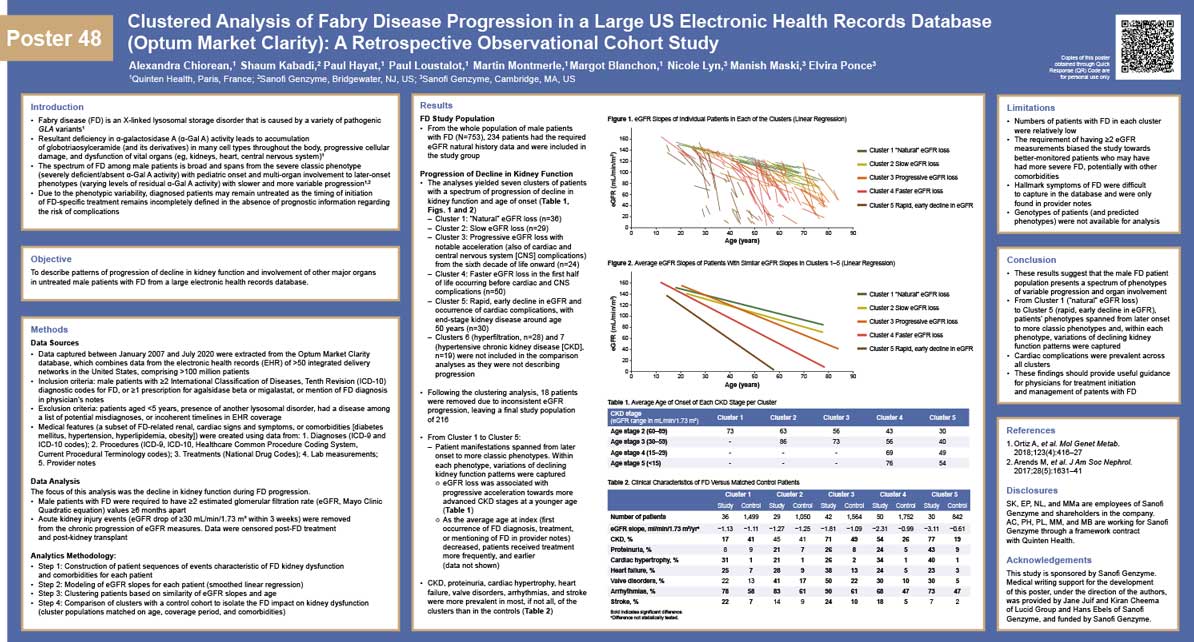
As the spectrum of Fabry phenotypes remains uncertain, the study objective was to describe patterns of progression in untreated Fabry disease (FD) patients from a large electronic health records database between January 2007-July 2020. Male patients with ICD-10 diagnostic codes for FD, prescriptions for agalsidase beta/migalastat, or mentions of FD diagnosis in physician’s notes were eligible for inclusion. Patients were excluded if younger than 5,had another lysosomal disorder,or another potential misdiagnoses.
OBJECTIVES:
Patients meeting eligibility criteria were in the Global FD Population (n=753). The focus of this analysis is on FD patients with at least 2 eGFR values 6 months apart prior to diagnosis (n=234). Speed of progression was measured using eGFR slopes with AKI events removed, with data censored post-FD treatment and post kidney transplant. FD patient progressions were clustered with a hierarchic agglomerative clustering algorithm on the combination of eGFR slope and extrapolated ages at CKD stage 2 and end stage renal disease.
PATIENT & METHODS:
The analyses yielded 7 clusters of patients with a spectrum of renal progression, including natural eGFR loss (n=36), slow eGFR loss (n=29), progressive eGFR loss (n=24), faster eGFR loss (n=50), rapid decline of eGFR (n=30), hyperfiltration (n=28), and hypertensive CKD (n=19). Each cluster was additionally described with statistics on the appearance of cardiac manifestations (e.g.,myocardial infarction), neurological manifestationsand classic FD hallmarks (e.g.,acroparesthesia). Further, progression in each cluster was compared with a control population matched on age, gender, coverage, and relevant comorbidities.
RESULTS:
Our results suggest that the male FD population expresses a spectrum of phenotypes and progressions. Within this spectrum, most identified FD patients experienced organ involvement relative to matched control patients, often leading to potentially irreversible organ damage such as chronic kidney injury.
CONCLUSIONS:
These findings should provide useful guidance for physicians on the selection of patients for initiation of FD treatments.